Hospital emergency? Study says Highland in danger of closure; Stockstill says data outdated
Published 7:00 am Saturday, November 14, 2015

NEW STUDY: Highland Community Hospital in Picayune is one of nine rural hospitals in Mississippi at greatest risk for closure based on a study conducted by the Social Science Research Center at Mississippi State University. Photo by Ashley Collins.
Highland Community Hospital is one of nine Mississippi hospitals that are at-risk of closure based on a study conducted by researchers from the Social Science Research Center at Mississippi State University.
“The Economic Impact of Potential Closures of Rural Hospitals in Mississippi,” was released in August and commissioned by the Center for Mississippi Health Policy to examine the economic impact of rural hospitals and their communities. It includes data from the American Hospital Association collected from 2008 to 2012, said Dr. Maya McDoom, the study’s lead researcher at MSU.
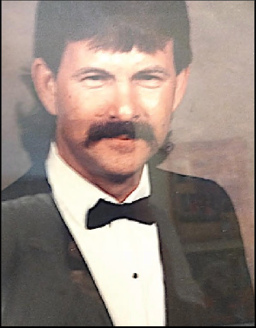
Highland Community Hospital Administrator Mark Stockstill said the hospital is far from being “at risk” these days.
Trending
“We’re not in danger of closing, we’re not about to close. We’re actually looking at a much brighter economic future,” Stockstill said.
McDoom said the hospitals were defined as “at risk” based on their profitability, uncompensated care and Medicaid shortfalls. At-risk hospitals are considered to be so financially vulnerable that they are at risk of closure because of money-losing decisions made internally or unexpected external events.
“We wrote this report not to say there’s a problem, but to work towards solutions that could sustain and help hospitals stay open,” McDoom said.
Stockstill said the time frame in which the data was collected, between 2008 to 2012, was a tough economic time nationwide. He also said the hospital, which is owned by Forrest Health, moved in July 2012 to the new facility on Highland Parkway and “the fiscal year ended from that data standpoint at the end of September, so we only had two months roughly of that 2012.”
In the old facility, Stockstill said they were seeing an average of 45 patients a day in the emergency room compared to the 65 to 90 patients they see at the new facility, which has been open for the past three years.
The “at risk” hospitals listed in the report include Highland Community Hospital, Covington County Hospital, Holmes County Hospital & Clinics, Tippah County Hospital, Hardy Wilson Memorial Hospital, Montfort Jones Memorial Hospital, Natchez Regional Medical Center, Noxubee County General Hospital and Tallahatchie County General Hospital, according to the study.
Trending
Stockstill said since the data is older, “it could falsely put the hospital in a very negative light when things could’ve changed to the contrary and vise versa.”
McDoom said they have received complaints from hospital administrators regarding the older data shown in the study.
“Some of the complaints are that it’s not 2015 data. But we have to wait to get the data from the AHA, and every year business financial situations change,” McDoom said.
She also said the list could be different if the data was from 2015.
The economic impact analysis from the study determined that the closure of all nine “most at risk” hospitals would lead to a loss of an estimated 2,600 jobs, approximately $8.6 million in state and local tax revenue and a total economic impact of $289.2 million.
Hospitals have a huge economic impact in their communities, said Therese Hanna, executive director at the Center for Mississippi Health Policy.
“Hospitals are often the largest employer in their area, usually behind the school district. Healthcare wise, a lot serve as a safety net for their area and if they weren’t available, people would have to drive far to get services,” Hanna said.
Stockstill said the hospital, between 2013 to 2015, “gave away an estimated $21 million of care through charity and bad debt.”
“One of the biggest things is, we paid more than $46 million in labor, in salaries and wages, not benefits. We know more than 95 percent of our employees live in this general area so that money is infused right back into the economy,” Stockstill said.
The hospital currently employs an estimated 356 employees, including around 35 contract employees, Stockstill said.
According to the study, there are numerous external factors influencing why rural hospitals are struggling. Those factors include expiration of rural hospital programs, macroeconomic stressors from the 2008 financial crisis, small hospital size and lack of capital, expiration of rural hospital programs, population loss and the passage of the Affordable Care Act. While the passage of the act has reduced the number of uninsured in Mississippi, hospitals are struggling to meet the requirements, such as adopting electronic medical records and coping with changes in reimbursement, the study stated.
One of the reimbursement issues is the reduction in Disproportionate Share Hospital payments program that partially compensates hospitals for providing care for the uninsured. Under the ACA, the DSH payments will be reduced as the Medicaid expansion is implemented. However, states like Mississippi that haven’t opted to expand Medicaid, won’t have that coverage growth to offset DSH cuts, according to the study.
“Every hospital in the state is feeling a loss of the disproportionate share. It’s not bad this year, but it will get bad as it moves on,” Stockstill said.
In order to deal with that issue, Stockstill said they plan to watch their expenses and look at service and supply contracts.
“With our relationship, and us being owned by Forrest Health, there’s a tremendous amount of bond power, so with that comes the ability to negotiate some really great supply savings,” Stockstill said.
He said one of their biggest challenges is “outmigration.” He said in a lot of the rural areas, people don’t visit their local hospitals.
“They go to a tertiary care center because there’s a perception of better care or better services, so that’s something we have to compete with,” Stockstill said.
The study highlights the need for those “at risk” hospitals to remain open for both economic and health benefits for their respective communities.
“The findings suggest that although rural hospitals in Mississippi face a host of challenges, there is also ample opportunity for hospitals to leverage a broad base of federal and state initiatives and self-help actions that ensure rural communities can meet the health needs of their local populations,” the study said.
Pearl River County Hospital and Nursing Home wasn’t involved in the study.